Health & Wellness
Sickle Cell Disease: FDA Approves New Gene Therapy Treatments
By Mary Alice Miller
The U.S. Food and Drug Administration has approved two new cell-based gene therapies for the treatment of sickle cell disease in patients 12 years and older. One of the new treatments, Casgevy, is the first FDA-approved treatment to utilize a novel type of genome editing technology. The other, Lyfgenia, is a cell-based gene therapy that modifies the patient’s blood stem cells to reduce the risk of blocked blood flow due to sickle-shaped blood cells.
Prior to these new treatments, the only therapy to treat sickle cell disease was a stem cell transplant that replaces bone marrow affected by sickle cell anemia with healthy bone marrow from a donor. A matching donor is usually a sibling who does not have sickle cell anemia. Other treatments revolved around pain management and prevention of crisis.
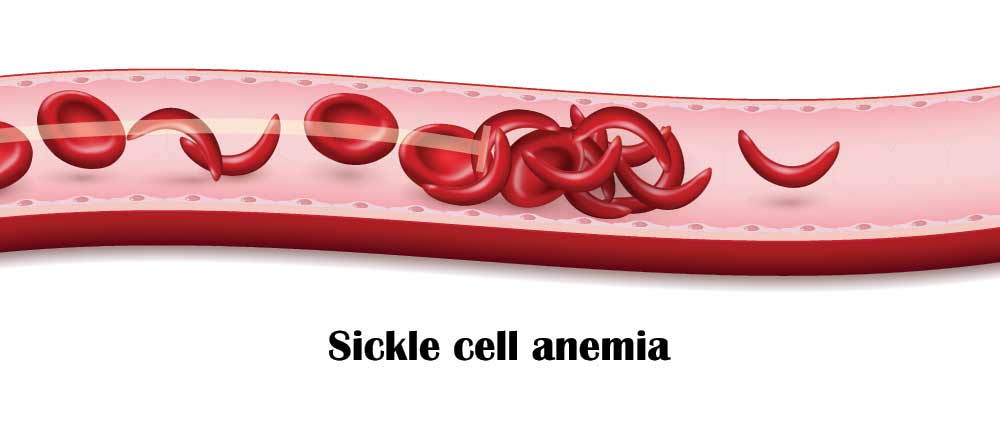
Sickle cell disease is an inherited blood disorder that is a mutation of hemoglobin, a protein found in red blood cells that deliver oxygen to the body’s tissues. The mutation causes red blood cells to develop a crescent or “sickle” shape. Sickled red blood cells restrict flow in blood vessels and limit oxygen delivery to the body’s tissues, leading to severe pain and organ damage. Recurrence of these events can lead to life-threatening disabilities and/or early death.
The National Institutes of Health (NIH) estimates sickle cell disease affects approximately 100,000 people in the U.S. It is most common among African Americans but also affects Hispanic Americans. About 1 in 13 Black or African American babies is born with sickle cell trait. Sickle cell disease occurs among about 1 in every 365 Black or African American births and about 1 in every 16,300 Hispanic American births.
The Centers for Disease Control and Prevention states that sickle cell disease occurs most often among people from parts of the world where malaria is or was common. People who carry the sickle cell trait are less likely to have severe forms of malaria.
According to the NIH, about 90% of the world’s sickle cell disease population lives in Nigeria, India, and the Democratic Republic of Congo.
Public awareness of sickle cell disease became widespread in 2017 when rapper Prodigy died while hospitalized from complications related to sickle cell anemia. Prodigy, raised in LeFrak City in Queens, was one half of the hip hop duo Mobb Deep.
Just last month the NYC Council passed a bill sponsored by Council Member Mercedes Narcisse that establishes a collaboration between the Department of Mental Health and Hygiene and New York City Health and Hospitals. That collaboration would develop guidelines with a structured approach to educate both medical professionals and the public on detecting sickle cell disease, and ensuring patients receive unbiased pain management.
Dr. Kusum Viswanathan, Chair of the Department of Pediatrics at Brookdale Hospital Medical Center, told Our Time Press, “The comprehensive sickle cell programs at One Brooklyn Health’s Brookdale Hospital Medical Center and Interfaith Medical Center take care of patients with sickle cell disease and follow them lifelong.
“They follow them in the outpatient program setting as inpatients, administer outpatient transfusions and pain management as needed, ensure that patients have access to the latest therapies, and educate and empower patients to achieve their goals. This approach has greatly reduced morbidity and mortality.
The Sickle Cell Society provides the following information on the inheritance of sickle cell anemia:
Everyone has two copies of the hemoglobin gene in every cell of their body; they get one from their mother and one from their father. Sickle cell anemia is called a recessive condition because you must have two copies of the sickle hemoglobin gene to have the disorder. If you have only one copy of the sickle hemoglobin along with one copy of the more usual hemoglobin you are said to have sickle cell trait. This is not an illness but means that you “carry” the gene and can pass it on to your children. If your partner also has sickle cell trait or sickle cell anemia your children could get sickle cell anemia.
If one parent has sickle cell trait and the other does not carry the sickle hemoglobin at all then none of the children will have sickle cell anemia. There is a one in two (50%) chance that any given child will get one copy of the sickle hemoglobin gene and therefore have the sickle cell trait. It is equally likely that any given child will get two usual hemoglobin genes and be completely unaffected.
If both parents have sickle cell traits, there is a one-in-four (25%) chance that any given child could be born with sickle cell anemia. There is also a one in four chance that any given child could be completely unaffected. There is a one in two (50%) chance that any given child will get sickle cell trait.
If one parent has sickle cell trait and the other has sickle cell anemia there is a one in two chance (50%) that any given child will get sickle cell trait and a one in two chance that any given child will get sickle cell anemia. No children will be completely unaffected.
If one parent has sickle cell anemia and the other is completely unaffected then all the children will have sickle cell trait. None will have sickle cell anemia. The parent who has sickle cell anemia can only pass the sickle hemoglobin to each of their children.













